- Research
- Open access
- Published:
Abdominal symptoms during Sjogren’s syndrome: a pilot study
Advances in Rheumatology volume 61, Article number: 5 (2021)
Abstract
Background
Abdominal symptoms in patients with primary Sjögren syndrome (pSS) are poorly documented. The objective of the study was to describe the abdominal symptoms of patients with pSS and to assess their association with characteristics of the disease.
Methods
One hundred and fifty patients with pSS were evaluated using a composite global symptom score for abdominal symptoms and their severity. Data concerning the clinical and biological characteristics of pSS and abdominal disorders were also collected.
Results
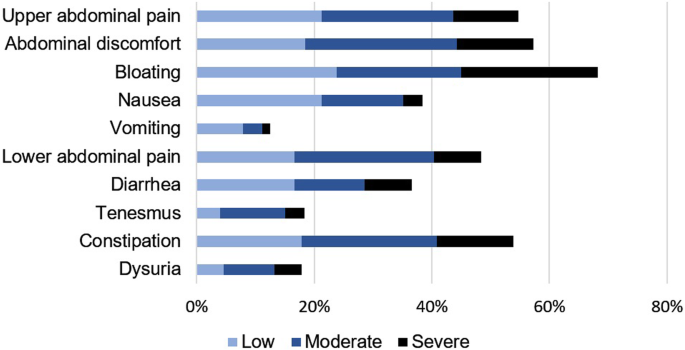
Of the patients with pSS, 95% suffered from abdominal symptoms (median global symptom score 7.5 ± 5.5 points out of 30). More than half of the patients experienced abdominal tension (68%), upper abdominal pain (54%), abdominal discomfort (58%) and/or constipation (54%). Regarding the pSS activity, in relation to European League Against Rheumatism (EULAR) Sjögren syndrome disease activity index score items, general and central nervous system involvement wereassociated with a high global symptom score. The EULAR Sjogren Syndrome Patient Reported Index (ESSPRI) symptom score was positively correlated with the global symptom score (p < 0.01). Multivariate analysis showed a significant association between a high global symptom score and SSA seronegativity, gastroparesis, and ESSPRI score (p < 0.01 for each).
Conclusions
The majority of patients with pSS suffered abdominal symptoms. There is currently no therapeutic recommendation because of the lack of information on the underlying pathophysiological mechanisms.
Trial registration
NCT03157011. Date of registration: July 17, 2017.
Background
Primary Sjögren syndrome (pSS) is a chronic autoimmune disorder characterized by lymphocytic infiltration of the exocrine glands and loss of secretory function with oral and ocular dryness. It affects predominantly females (female:male ratio 9:1), and the peak frequency of the disease is about age 50 years. The etiology of pSS is unclear [1]. Like other autoimmune diseases, negative impact, pain, and fatigue predominate, reducing the quality of life. Furthermore, abdominal disorders affect approximately 25% of patients with pSS but are poorly documented in the literature [2]. Indeed, epidemiological characteristics vary among studies because of the small number of patients and use of old classification criteria [2]. Also, data concerning the frequency of abdominal symptoms and their associations with clinical and biological manifestations of pSS are contradictory [2]. This heterogeneity led us to conduct a non-interventional prospective study of abdominal symptoms in patients with pSS as defined by the 2016 American College of Rheumatology-European League Against Rheumatism (ACR-EULAR) criteria [3].
Methods
Population
From July 2017 to June 2018, we conducted a single-center study in a French Hospital and University Center. It was a prospective, non-interventional study, and was approved by the Committee for the Protection of Individuals “Sud-Ouest et Outre Mer III” (France). All patients (age > 18 years) followed in our center for pSS were considered for enrollment. All of them fulfilled the 2016 ACR-EULAR classification criteria for pSS [3]. The patients provided written consent after receiving information on the study. The patients’ characteristics (age at disease onset, sex, and duration of pSS), clinical manifestations of pSS, associated organ-specific autoimmune disorders, and treatments were recorded. pSS Activity as measured by the EULAR Sjögren syndrome disease activity index (ESSDAI) and pSS symptoms measured by EULAR Sjogren Syndrome Patient Reported Index (ESSPRI) were systematically evaluated concurrently with abdominal symptoms [4]. The data were completely anonymized before being assessed. Blood tests were performed at the time of diagnosis and concurrently with assessment of the abdominal symptoms score.
Evaluation of abdominal symptoms
The patients with pSS were interviewed by a physician using a questionnaire. The questionnaire comprised 10 abdominal symptoms (nausea, vomiting, upper and lower abdominal pain, abdominal discomfort, bloating, diarrhea, constipation, tenesmus, dysuria). Each symptom was scored from 0 (no symptom) to 3 (severe) as evaluated by professional judgement. A global symptom score (GSS), calculated as the sum of all symptom scores, was assigned to each patient (maximum score, 30) [5,6,7,8,9,10,11,12,13]. This score has been used for another chronic autoimmune disease, systemic sclerosis, as well as for two chronic digestive pathologies (i.e., diverticulitis and functional dyspepsia) [5,6,7,8,9,10,11,12,13]. Previously diagnosed digestive, pancreatic, and hepatic diseases, as well as treatments for digestive complaints, were systematically recorded in the medical file. Previous diagnosis of gastroparesis was based on international clinical guidelines [14] and irritable bowel syndrome on the Rome IV classification [15]. After completing the questionnaire, only those patients with alarm signs (endoscopy) or signs evocative of gastroparesis (gastric emptying scintigraphy) underwent exploration of the digestive system, in accordance with the French recommendations [16,17,18].
Statistical analysis
Quantitative variables are presented as means ± standard deviations, and qualitative variables as numbers and percentages. For qualitative variables, a chi-squared or Fisher’s exact test was used to compare the groups (SSA +/− SSB patients and seronegative patients). For normally distributed quantitative variables, Student’s t-test was used to compare groups of two or more classes. For non-normally distributed quantitative variables, the Wilcoxon signed-rank test or the Kruskal–Wallis test was used to compare groups of two or more classes. Univariate analyses between the abdominal symptoms and the other variables were performed. Variables with a value of p < 0.20 were included in a multivariate logistic model, simplified by a stepwise elimination method [19], so that the final model included only variables significantly associated with digestive symptoms. Quantitative variables fulfilling the logit linearity assumption were incorporated without modification, or otherwise categorized. The relevance of the model was assessed using Pearson’s residual and deviance tests, and its quality by means of a receiver operating characteristic curve. To test the correlation between the GSS score and continuous variables, Spearman’s rho was calculated. A supervised discretization will be performed with a decision tree to identify thresholds for the GSS variable. Statistical analysis was conducted using R software (version 3.2.2, rpart package). Values of p < 0.05 were considered indicative of significance.
Results
Patients’ characteristics and treatments
A total of 150 patients (mean age 63 ± 13 years, male n = 9) with pSS were enrolled. Eighty patients (53%) had anti-SSA antibodies and 31 (21%) had anti-SSB antibodies (22%). One hundred and four patients (86%) had a Chisholm score of ≥3 at the time of diagnosis. None of the patients had auto-antibodies, symptoms, or capillaroscopy findings suggestive of an associated systemic sclerosis. The most common systemic involvements, defined in the ESSDAI score, were articular (n = 107; 71%) and muscular (n = 68; 45%). Twenty-two percent of the patients (n = 33) had neurological involvement (central n = 20 [13%] and/or peripheral n = 24 [16%] with 14 [9%] biopsy-proven small-fiber neuropathies) [20]. Other systemic involvements were hematologic (n = 30; 20%), pulmonary (n = 17; 11%), cutaneous vasculitis (n = 11; 7%) and interstitial nephritis (n = 8; 5%) (Table 1). The average ESSDAI score was 3.4 ± 4.8 points out of 123. The average ESSPRI score was 5.9 ± 2.1 out of 10. The latter score is the average of the dryness (6.2 ± 2.4 out of 10), fatigue (6.2 ± 2.4) and pain (5.5 ± 2.7) scores. Hydroxychloroquine was taken by 46% (n = 70) of the patients, corticosteroids by 23% (n = 35), immunosuppressive drugs by 14% (n = 22; including three patients taking mycophenolate mofetil), targeted therapies by 3% (n = 5), and intravenous immunoglobulin by 5% (n = 8). Symptomatic treatments included standard analgesics (n = 51; 34%), specific neuropathic pain treatments (n = 26; 17%), and nonsteroidal anti-inflammatory drugs (n = 13; 8%). Seventeen percent of the patients (n = 26) used antidepressants and 15% (n = 23) used benzodiazepines.
Previous digestive disease
Forty-four patients had symptomatic gastroesophageal reflux (29%). Thirteen patients had at least one gastric emptying scintigraphy for clinical signs suggestive of gastroparesis (9%); among them, nine had a confirmed gastroparesis. Of these nine patients, three had mild, three had moderate, and three had severe gastroparesis, according to the fixation rate at 4 h6. All of the patients received medical treatment, three patients received botulinum toxin injections, and two underwent endoscopic pylorotomy. Only 7 patients (4.7%) had diabetes mellitus, none of whom had gastroparesis. Another 7 patients had autoimmune hepatitis with 4 cases of primary biliary cholangitis and 3 of sclerosing cholangitis. Twenty-seven cases of gastritis (18%), mostly atrophic, were reported, as well as three cases of pernicious anemia (2%) and one of coeliac disease. Thirty cases of irritable bowel syndrome were documented (20%). Sixteen patients had enteric endoscopic diverticulosis (11%), which was complicated by diverticulitis in five patients. Three cases of dolichocolons were noted. Forty-eight percent of the patients had used at least one treatment for abdominal symptoms in the previous 2 weeks. The most highly represented drug classes were proton pump inhibitors (n = 45; 30%), laxatives (n = 14; 9%), antispasmodics (n = 19; 13%), sodium alginates and/or coals (n = 11; 7%), ursodeoxycholic acid (n = 6; 4%), prokinetics (n = 5; 3%), and anti-diarrheals (n = 5; 3%).
Abdominal symptoms
Ninety-five percent of the patients (n = 143) suffered from abdominal symptoms (median GSS score = 7.5 ± 5.5 points). The abdominal complaints are shown according to severity in Fig. 1. More than half of the patients had upper abdominal pain, abdominal discomfort, bloating and/or constipation. Several features of pSS were associated with a GSS using a score higher than 10 obtained by supervised discretization (Table 2). There was no correlation between abdominal symptoms and focus score on minor salivary gland biopsy or unstimulated salivary flow.
Regarding the ESSDAI score items, articular involvement was associated with a GSS > 10. Muscular, pulmonary and neurological involvement were more present with a GSS > 10 but not significantly (Table 2).
The total ESSPRI score was correlated with the GSS score (0.48; Rho = 0.5, p < 0.0001). The three items of the ESSPRI score were also correlated with a high GSS score (dryness Rho = 0.3, p = 0.0014, fatigue Rho = 0.5, p < 0.0001 and pain Rho = 0.4, p < 0.0001).
Several digestive antecedents were correlated with a high GSS score: hiatal hernia (GSS = 12.4 ± 5.6 vs. 9.0 ± 6.1, p = 0.007), gastroesophageal reflux (GSS = 12.3 ± 6.1 vs. 8.7 ± 5.9, p = 0.001), gastroparesis (GSS = 15.9 ± 2.5 vs. 9.4 ± 6.1, p = 0.0032), atrophic gastritis (GSS = 15.1 ± 4.9 vs. 9.4 ± 6.1, p = 0.0097), irritable bowel syndrome (GSS = 13.4 ± 5.8 vs. 8.8 ± 5.9, p = 0.0002), at least one previous abdominal surgery (GSS = 13.4 ± 5.8 vs. 8.8 ± 5.9, p = 0.0440), and pernicious anemia (GSS = 19.0 ± 8.5 vs. 9.6 ± 6.0, p = 0.0306). Use of treatments for gastrointestinal symptoms was correlated with a high GSS (trimebutine [GSS = 15.6 ± 6.5 vs. 9.4 ± 6.0, p = 0.0047] and proton pump inhibitors [GSS = 12.4 ± 6.5 vs. 8.6 ± 5.6, p = 0.0004]). In addition, a high GSS score was correlated with a higher frequency of endoscopic explorations and gastric emptying scintigraphy (GSS = 14.6 ± 6.1 vs. 9.3 ± 6.0, p = 0.0037). No pSS-specific therapy was correlated with a high abdominal symptoms score. Serologic status influenced the overall abdominal score as well as the prevalence of several abdominal symptoms (Table 3). Indeed, the median GSS score was significantly higher in seronegative patients (GSS = 11.8 ± 5.8 vs. 7.9 ± 5.9, p = 0.02).
The multivariate analysis of the total GSS score (linear regression) and upper gastrointestinal symptoms (logistic regression) vs. patient characteristics is shown in Table 4. No item was significantly related to reduced abdominal symptoms in the multivariate analysis. The multivariate analysis confirmed the significant association between the GSS total score, ESSPRI score, and seronegativity (p < 0.01; Table 4). The fatigue and fever items of the GSS score were associated with seronegativity (OR = 8.45; p = 0.0152) and a high ESSPRI score (OR = 1.31; p < 0.0001).
Discussion
This study is the first to use the 2016 ACR-EULAR criteria to systematically evaluate the severity of abdominal symptoms in patients with pSS. Abdominal disorders are rarely reported during pSS and are probably underestimated [2]. The reported prevalence varies markedly depending on the pSS diagnostic criteria and the number of patients evaluated. Moreover, studies have typically focused on one type of abdominal involvement [2]. For example, Retamozo reported a 6.2% prevalence of abdominal disorders but evaluated only chronic gastritis, acute pancreatitis, and dysphagia [21]. We found a high frequency of major upper and lower abdominal complaints in patients with pSS.
These symptoms are likely to be responsible for deterioration in the quality of life of pSS patients. Indeed, Krogh et al. demonstrated that abdominal complaints were a source of impairment of quality of life for pSS patients [22]. However, the correlation between abdominal complaints and ESSPRI score has not been evaluated [22]. Our study showed a strong association between abdominal symptoms and a high ESSPRI score.
A retrospective Indian study showed clustering of gastrointestinal symptoms and depression/psychiatric symptoms in pSS, but only evaluated irritable bowel syndrome [23]. Although depressive symptoms were the most frequent in seronegative patients with pSS, they were not significantly associated with gastrointestinal symptoms.
Despite their frequency, digestive symptoms are not part of the ESSDAI activity score for pSS. Likewise, the ESSPRI score evaluating the frequent symptoms of pSS did not account for abdominal complaints. Almost half of the patients used treatments for digestive symptoms, which was correlated with a high abdominal score. This suggests that these treatments are ineffective and unsuitable for pSS with digestive involvement. Otherwise, pSS treatments did not influence abdominal symptoms, suggesting both their ineffectiveness and the absence of an exclusive adverse side effect that may explain such symptoms. Therefore, large prospective studies of the pathophysiology of these frequent symptoms are needed.
Dysfunction of the autonomic nervous system plays an important role in the pathogenesis of gastrointestinal manifestations of pSS. Autonomic neuropathy has been described in patients with pSS and is associated with orthostatic hypotension, urinary retention, segmental anhidrosis, and dysfunction of the digestive and urinary systems [24]. Muscarinic receptors M3 are expressed on vascular smooth muscle cells, particularly in the gastrointestinal and genitourinary systems, as well as on exocrine gland cells [25, 26]. In patients with pSS, autoantibodies are directed against muscarinic receptors [25], suggesting these antibodies to be the cause of autonomic neuropathy, which can lead to bladder insufficiency or gastrointestinal disorders [26]. Such autoantibodies were implicated in altered colonic contraction in an ex vivo model [27]. Intravenous immunoglobulin shows promise for the treatment of immunologically induced digestive or urinary disorders. Smith et al. showed that intravenous immunoglobulin neutralized anti-muscarinic M3 receptor antibodies and improved the urinary and diarrhea scores in a patient with pSS [28].
The multivariate analysis showed an association between a high abdominal symptom score and a prior diagnosis of gastroparesis. Gastroparesis is likely to be underdiagnosed in patients with pSS. We found a 69% rate of confirmed gastroparesis among patients who underwent emptying gastric scintigraphy to explore symptoms suggestive of this condition. Few studies have evaluated gastroparesis during pSS [25, 29, 30]. Kovacs et al. reported a 70% rate of scintigraphy-proven gastroparesis in 30 symptomatic patients with pSS [25]. Another study of 28 patients with pSS found a prevalence of 43% for subjective signs of gastroparesis and 29% for gastroparesis confirmed by octanoate breath tests [29]. In a retrospective study of 11 patients with pSS-associated gastroparesis, 82% had bloating and abdominal pain [30]. The relationship between gastroparesis and involvement of the autonomic nervous system in pSS is unclear. Such a relationship is hypothesized based on inhibition of gastric emptying by anti-muscarinic receptor type 3 antibodies [25]. Unfortunately, no study has evaluated the correlation of the level of these antibodies with the gastric emptying time. Our findings suggest the necessity of excluding gastroparesis in the presence of unexplained persistent upper digestive symptoms in a patient with pSS.
This study had several limitations. The GSS is based on a questionnaire that is easy to use in routine practice with patients, but it is a non-validated tool. We did not evaluate abdominal symptoms in a healthy patient cohort. It is a preliminary study mainly to highlight the presence of these symptoms in a cohort of Sjögren’s patients and to evaluate their relationship to disease activity (ESSDAI) and to the most frequent symptoms (ESSPRI). This exploratory study included only patients attending a single university hospital center, which could have resulted in selection bias. However, the prevalence of systemic involvement was consistent with the findings of other French pSS studies [31, 32]. The non-interventional study design precluded demonstration of a causal link between digestive symptoms and pSS. Also, we did not systematically investigate digestive symptoms by endoscopy, which may have led to their mis- or under-diagnosis. Regarding the hypothetical link between gastrointestinal involvement and autonomic neuropathy, we did not perform physiological testing, quantitative measurement of autonomic nervous system function, or assays of anti-muscarinic receptor antibodies.
The chief strength of this study was its evaluation of a simple and rapid tool to screen and assess digestive symptoms among a large cohort of pSS patients. The majority of patients with pSS had abdominal complaints that affected their quality of life. Therefore, the questionnaire could enable not only detection but also monitoring of abdominal complaints over time. Furthermore, the questionnaire was capable of diagnosing gastroparesis, a poorly described, potentially debilitating condition associated with pSS.
Conclusion
We detected gastrointestinal symptoms in the majority of patients with pSS. Prospective studies are needed to clarify the relationship between abdominal complaints and depressive disorders and/or fibromyalgia, and investigate the underlying pathophysiological mechanisms.
Availability of data and materials
The data were completely anonymized before being accessed by the authors.
References
Qin B, Wang J, Yang Z, Yang M, Ma N, Huang F, et al. Epidemiology of primary Sjögren’s syndrome: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74:1983–9.
Ebert EC. Gastrointestinal and hepatic manifestations of Sjogren syndrome. J Clin Gastroenterol. 2012;46:25–30.
Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, et al. 2016 American College of Rheumatology/European league against rheumatism classification criteria for primary Sjögren’s syndrome: A consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheum. 2017;69:35–45.
Seror R, Theander E, Brun JG, Ramos-Casals M, Valim V, Dörner T, et al. Validation of EULAR primary Sjögren’s syndrome disease activity (ESSDAI) and patient indexes (ESSPRI). Ann Rheum Dis. 2015;74:859–66.
Marie I, Gourcerol G, Leroi AM, Ménard JF, Levesque H, Ducrotté P, et al. Delayed gastric emptying determined using the 13C-octanoic acid breath test in patients with systemic sclerosis. Arthritis Rheum. 2012;64:2346–55.
Latella G, Pimpo M, Sottili S, Zippi M, Viscido A, Chiaramonte M, et al. Rifaximin improves symptoms of acquired uncomplicated diverticular disease of the colon. Int J Color Dis. 2003;18:55–62.
Di Mario F, Aragona G, Leandro G, Comparato G, Fanigliulo L, Cavallaro LG, et al. Efficacy of mesalazine in the treatment of symptomatic diverticular disease. Dig Dis Sci. 2005;50:581–6.
Di Mario F, Stefani N, Dal Bò N, Rugge M, Pilotto A, Cavestro GM, et al. Natural course of functional dyspepsia after helicobacter pylori eradication: a seven-year survey. Dig Dis Sci. 2005;50:2286–9.
Marie I, Leroi AM, Gourcerol G, Levesque H, Menard JF, Ducrotte P. Lactose malabsorption in systemic sclerosis. Aliment Pharmacol Ther. 2016;44:1123–33.
Gemignani L, Savarino V, Ghio M, Parodi A, Zentilin P, de Bortoli N, et al. Lactulose breath test to assess oro-cecal transit delay and estimate esophageal dysmotility in scleroderma patients. Semin Arthritis Rheum. 2013;42:522–9.
Marie I, Ducrotté P, Denis P, Menard JF, Levesque H. Small intestinal bacterial overgrowth in systemic sclerosis. Rheumatology. 2009;48:1314–9.
Parodi A, Sessarego M, Greco A, Bazzica M, Filaci G, Setti M, Savarino E, Indiveri F, Savarino V, Ghio M, Parodi A, et al. Small intestinal bacterial overgrowth in patients suffering from scleroderma: clinical effectiveness of its eradication. Am J Gastroenterol. 2008;103:1257–62.
Marie I, Antonietti M, Houivet E, Hachulla E, Maunoury V, Bienvenu B, et al. Gastrointestinal mucosal abnormalities using videocapsule endoscopy in systemic sclerosis. Aliment Pharmacol Ther. 2014;40:189–99.
Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L. American College of Gastroenterology. Clinical guideline: management of gastroparesis. Am J Gastroenterol. 2013;108:18–37.
Palsson OS, Whitehead WE, van Tilburg MA, Chang L, Chey W, Crowell MD, et al. Development and validation of the Rome IV diagnostic questionnaire for adults. Gastroenterology. 2016;150:1481–91.
Carayon P. Guidelines of the French Society of Digestive Endoscopy: total colonoscopy indications. The Council of the French Society of digestive endoscopy (SFED). Endoscopy. 2000;32:434–5.
https://www.has-sante.fr/portail/upload/docs/application/pdf/gastro_endoscopy.pdf.
Couturier O, Victor G, Faivre-Chauvet A, Baulieu F, Le Rest C, Bridji B, et al. Guide de bonnes pratiques en scintigraphie de la vidange gastrique. Méd Nucl. 2002;26:211–9.
Harrell F. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. New York: Springer; 2001.
Chai J, Herrmann DN, Stanton M, Barbano RL, Logigian EL. Painful small-fiber neuropathy in Sjogren syndrome. Neurology. 2005;65:925–7.
Retamozo S, Acar-Denizli N, Rasmussen A, Horváth IF, Baldini C, Priori R, et al. Systemic manifestations of primary Sjögren's syndrome out of the ESSDAI classification: prevalence and clinical relevance in a large international, multi-ethnic cohort of patients. Clin Exp Rheumatol. 2019;37:97–106.
Krogh K, Asmussen K, Stengaard-Pedersen K, Laurberg S, Deleuran BW. Bowel symptoms in patients with primary Sjögren's syndrome. Scand J Rheumatol. 2007;36:407–9.
Sandhya P, Jeyaseelan L, Scofield RH, Danda D. Clinical characteristics and outcome of primary Sjogren's syndrome: A large Asian Indian cohort. Open Rheumatol J. 2015;9:36–45.
Pavlakis PP, Alexopoulos H, Kosmidis ML, Mamali I, Moutsopoulos HM, Tzioufas AG, et al. Peripheral neuropathies in Sjögren's syndrome: a critical update on clinical features and pathogenetic mechanisms. J Autoimmun. 2012;39:27–33.
Kovács L, Papós M, Takács R, Róka R, Csenke Z, Kovács A, et al. Autonomic nervous system dysfunction involving the gastrointestinal and the urinary tracts in primary Sjögren’s syndrome. Clin Exp Rheumatol. 2003;21:697–703.
Goodman BP, Crepeau A, Dhawan PS, Khoury JA, Harris LA. Spectrum of autonomic nervous system impairment in Sjögren syndrome. Neurologist. 2017;22:127–30.
Park K, Haberberger RV, Gordon TP, Jackson MW. Antibodies interfering with the type 3 muscarinic receptor pathway inhibit gastrointestinal motility and cholinergic neurotransmission in Sjögren's syndrome. Arthritis Rheum. 2011;63:1426–34.
Smith AJ, Jackson MW, Wang F, Cavill D, Rischmueller M, Gordon TP. Neutralization of muscarinic receptor autoantibodies by intravenous immunoglobulin in Sjögren syndrome. Hum Immunol. 2005;66:411–6.
Hammar O, Ohlsson B, Wollmer P, Mandl T. Impaired gastric emptying in primary Sjogren’s syndrome. J Rheumatol. 2010;37:2313–8.
Geyl S, Jacques J, Parreau S, Cypierre A, Tabouret T, Gondran G, et al. Gastroparesis may be the cause of unexplained dyspepsia in patients with primary Sjögren syndrome. Rev Med Interne. 2018;39:427–30.
Martel C, Gondran G, Launay D, Lalloué F, Palat S, Lambert M, et al. Active immunological profile is associated with systemic Sjögren’s syndrome. J Clin Immunol. 2011;31:840–7.
Carvajal Alegria G, Guellec D, Mariette X, Gottenberg JE, Dernis E, Dubost JJ, et al. Epidemiology of neurological manifestations in Sjögren's syndrome: data from the French ASSESS cohort. RMD Open. 2016;20:e000179.
Acknowledgements
None.
Funding
The work was not funded.
Author information
Authors and Affiliations
Contributions
Each named author has substantially contributed to the research and/or drafting of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study were in accordance with the ethical standards of the Institutional Research Committee and with the 1964 Helsinki Declaration and its later amendments. The study was approved by the Committee for the Protection of Individuals “Sud-Ouest et Outre Mer III” (France). All patients provided written consent after receiving information about the study.
Consent for publication
All patients provided written consent after receiving information about publication.
Competing interests
The authors declare no conflict of interest.
Provided written consent after receiving information about the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Parreau, S., Jacques, J., Dumonteil, S. et al. Abdominal symptoms during Sjogren’s syndrome: a pilot study. Adv Rheumatol 61, 5 (2021). https://doi.org/10.1186/s42358-021-00164-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-021-00164-w